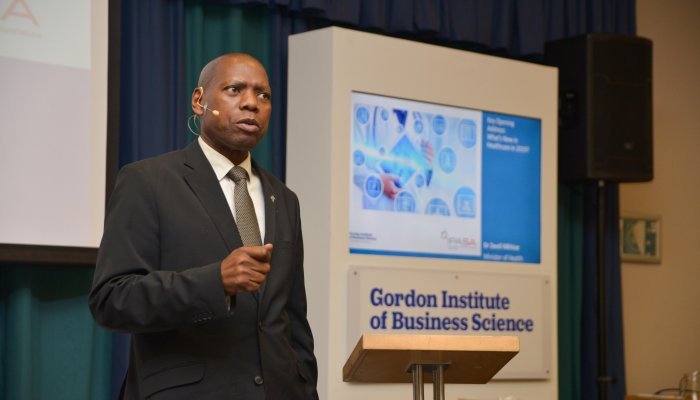
The National Health Insurance (NHI) Bill was tabled in parliament at the beginning of August 2019 for public consultation signalling government’s intention to roll out South Africa’s answer to Universal Healthcare Coverage (UHC) by 2026. Despite having been in motion for 11 years, NHI remains highly contentious among stakeholders in healthcare, especially those in the private sector who are unclear about their role and future. The GIBS/IPASA Health Industry Insights 2019 Conference, headlined by Health Minister Dr. Zweli Mkhize together with leaders representing different stakeholders in the healthcare value chain, sought to provide answers to this NHI debate and forge a way forward.
...prioritising the sick and the elderly over their healthier counterparts...
Responding to questions in parliament on NHI, President Cyril Ramaphosa related an anecdote told by the late Swedish prime minister Olof Palme about an earlier prime minister who shared a hospital ward with a steelworker and received the same care as him through that nation’s UHC. Ramaphosa envisioned the same democratisation of healthcare services being achieved in South Africa through the implementation of the NHI.
Yet, unlike Sweden – and other OECD countries – South Africa is one of the most unequal societies in the world. That inequality is stark when it comes to healthcare. Ramaphosa said that approximately R250 billion is spent annually on the 16% of the population that has access to private healthcare, while about R220 billion covers public healthcare that is accessed by the majority.
Speaking at the GIBS conference, Mkhize presented NHI as ‘a system that will allow all South Africans access to healthcare whether they are poor, unemployed, rich or don’t have medical aid’. He said NHI was based on social solidarity where all South Africans would put their resources together, prioritising the sick and the elderly over their healthier counterparts.
“The proposal that we are working on was based on the United Nations and the World Health Organisation as part of ensuring access to healthcare. It is based on a number of OECD countries who have achieved UHC. It means we must open up healthcare services to allow people into the system. The one who needs a heart transplant must go through the system and not be stopped because they cannot afford to have such an operation,” explained Mkhize.
Current state of public healthcare
As it currently stands, public healthcare, which is accessed by the majority of South Africans – mainly black Africans – desperately needs overhauling. Sick people must contend with long queues, poor facilities and demotivated staff, limited access to doctors and specialists, and are often sent home with no medicine as district and provincial health facilities run out of budgets.
...some government hospitals were ‘becoming mortuaries instead of sanctuaries for saving lives’....
Delivering his budget vote speech, Gauteng premier David Makhura admitted that the public health system faced a crisis of public confidence and that some government hospitals were ‘becoming mortuaries instead of sanctuaries for saving lives’, further conceding that government needed to fix these urgently.
The Life Esidimeni tragedy, which resulted in the death of 143 patients in psychiatric facilities in Gauteng in 2016, continues to be a leading example of a state that is struggling to care for its citizens. Cases of medical negligence at state facilities are alarming. Figures from 2017 show that the Gauteng provincial health department was leading with a bill of R18.6 billion in negligence claims followed by the Eastern Cape with R16.7 billion and KZN with over R9.2 billion.
NHI will be implemented in three phases over a period of 14 years beginning in 2026. The fund will buy or procure medical healthcare – from primary healthcare to highly specialised care – on behalf of all South Africans. The South African Revenue Service will collect funds from all sources of revenue identified by National Treasury to purchase and reimburse accredited and contracted providers, and private and public healthcare facilities will be required to be world-class.
“The quality of healthcare in government-run facilities must improve to make the public sector a service of choice in terms of access, affordability, availability and appropriateness, technical competence, skills, effectiveness, efficacy, respect and caring amongst others,” revealed Mkhize.
He also promised that clinics and hospitals would be adequately staffed with well-trained healthcare workers and have a sufficient supply of medicine and vaccines to meet the demand.
“NHI must not be considered as wasteful expenditure but an investment in human capital development, a healthier population, and economic growth, and it is out of that investment that we will be able to build on the prosperity of the country,” pleaded Mkhize.
Mkhize emphasised that government would swiftly address maladministration, incompetence and corruption. He also said they would tap into expertise gleaned from private healthcare to manage the fund, which will be complex.
Marius Oosthuizen, GIBS Faculty, accused government of selling ideologically-informed policy perspectives to the population and said NHI had the potential to be held up in litigation.
“At the end of the day, you can have all the fancy policies, but if you don’t fix the leaks, you are going nowhere. If the minister came today and said we are going to have a campaign to fix the system for five to 10 years, focused on fixing governance and delivery of healthcare in our clinics and hospitals, training people and monitoring effectively, delivering services at a world-class standard with the resources we have - and invited the private sector – we would all jump up and be behind the minister,” said Oosthuizen.
“What we need is much more participative democracy, co-creation of policy, and more dialogue and engagement at a substantive level to say what are the realities on the ground – it requires pragmatism and to say how can we achieve better healthcare using what is in the public and what is in the private sector,” he added.
Governance
NHI will be managed by a Schedule 3 entity under the Public Finance Management Act and receive all its revenue from the fiscus. Its mandate will be to spend on the designated services. The minister will appoint the 11-person board, one of whom will represent the health minister, to oversee the implementation of the NHI fund. The board, which will be accountable to the health minister, will be responsible for appointing the fund's CEO.
Also speaking at the GIBS conference was Dr Lance Lasersohn, Specialist Anesthesiologist and Intensive Care Physician, SASA Vice President (President-Elect), who called for more regulation.
“The lack of regulation is a big problem. The minister will be a ruler in totality and will not be regulated by an outside body. It is flawed. Our lived experience is that we can’t trust [government]. We’ve been exposed to maladministration and corruption and it’s hard to negotiate with people you can’t trust. Once government can demonstrate trust, we can go far,” said Lasersohn.
Building trust
During the conference, stakeholders supported the government’s efforts to afford all South Africans access to UHC. However, the bone of contention was the unclear framework of how NHI would be implemented, inadequate consultation and lack of clarity on the role of the private sector to make it possible. Government’s failure to manage state funds as demonstrated in the currently dysfunctional public health sector was cited as a barrier.
Dr Vusi Nhlapo, GM of South African Medical Association (SAMA), which represents almost 17 000 doctors, said further engagement was needed with the government on a variety of issues concerning NHI.
“There isn’t a clear idea of what provincial health departments will be doing. We know that there is thinking that the district health management system will be taking over some of the functions. That concerns doctors because if you look at what happened in the past, doctors would provide a service and not get paid for it. Trust deficit needs to be fixed and we need honest and robust discussions that will get to the granular details and earn trust,” said Nhlapo.
Role of medical schemes
There has been speculation that the implementation of NHI will result in the end of medical aid schemes and the loss of thousands of jobs.
Lerato Mosiah, CEO of the Health Funders Association, an industry body that represents 53% of the country’s medical aid schemes, administrations and managed care organisations, said they would continue to engage with the minister and his department for clarity.
“We support the government in all its endeavours to implement a universal health system and we have to implement it. Our concern is around the role of schemes in the NHI Bill. What does ‘complementary’ really mean?” asked Mosiah.
She further stated that medical aid schemes would not be obliterated by the NHI as was previously believed but wondered if customers would actually be able to afford them.
Discovery
Discovery Health, one of South Africa’s largest medical schemes, says it fully supported the drive to ensure that all South Africans have access to quality health services based on need rather than affordability and was also supportive of NHI.
In comments emailed to Acumen, Discovery Health CEO, Dr Jonathan Broomberg, says he wants clarity on the potential impact the NHI Bill would have on the future of private healthcare and medical schemes. Like Mosiah, Broomberg says Discovery also needs clarity from the department of health on the “complementary cover” that will be provided by schemes.
“Our strong view is that substantially limiting the role of medical schemes would be counterproductive to NHI because there are simply insufficient resources to meet the needs of all South Africans. Limiting people from purchasing the medical scheme coverage they need will seriously curtail their rights, and this could seriously impact the sustainability of private healthcare, as well as skills, the economy and sentiment,” says Broomberg, adding that Discovery would engage actively and constructively with government to ensure that medical schemes play an ongoing, critical role to the NHI process.
“We also think that once fully emerged, the NHI will create additional opportunities for medical schemes to innovate in their products and for the development of new health insurance products outside of the medical scheme environment,” adds Broomberg.
...once fully emerged, the NHI will create additional opportunities for medical schemes to innovate in their products...
What's next?
With the NHI Bill in parliament for public consultations, panellists at the GIBS conference urged South Africans to actively engage with the Bill and share their comment for consideration.
“The concept is a good one, but it is our ethical prerogative for each of us to go through the Bill,” said Lasersohn.
They further called on the government to establish more platforms for further engagement with all stakeholders and provide clarity on the NHI Bill in a bid to reach viable private/public partnerships.
“We need a more participative democracy, co-creation of policy, more dialogue and engagement at a substantive level. It requires pragmatism that says how we, as South Africans, can achieve better healthcare using what is in the public and the private sector. It will require a substantive partnership where stakeholders make a 10-15 year commitment to help the country,” implored Oosthuizen.